Lynch Syndrome is one of the most common causes of hereditary cancer, yet it remains a little-known disease. This genetic syndrome significantly increases the risk of developing several types of cancer, mainly colon and endometrial cancer. In this article, we will explore the crucial connection between genetics and Lynch Syndrome, explaining what it is, how it is inherited, and why genetic testing plays a fundamental role in the prevention, detection, and treatment of this condition. Patients, families, and healthcare professionals will be able to better understand this condition—a fundamental first step for people at risk.
What is Lynch Syndrome and why is it a hereditary cancer?
Lynch Syndrome, also known as Hereditary Nonpolyposis Colorectal Cancer (HNPCC), is a genetic disease that significantly increases a person’s risk of developing certain types of cancer, particularly colorectal and endometrial cancer. Unlike sporadic cases of cancer that arise without a clear cause, Lynch Syndrome is hereditary, meaning it is passed from parents to children through genetic mutations. It is important to note that carrying these mutations does not mean you will necessarily develop cancer—it only raises the risk of developing the disease.
The syndrome is named after Dr. Henry T. Lynch, who first described this disorder in the 1960s.
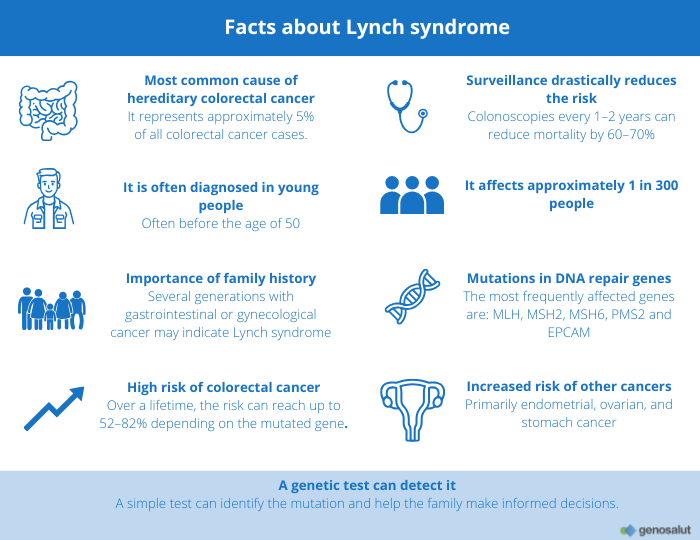
Understanding Lynch Syndrome is essential for early detection and treatment, as people with this disease are more likely to develop cancer at a younger age compared to the general population. The syndrome accounts for about 3–5% of all colorectal cancer cases, making it the most common form of hereditary colorectal cancer. However, Lynch Syndrome is not limited to colorectal cancer; it also predisposes people to other malignancies such as endometrial, ovarian, gastric, and urinary tract cancers, among others.
If colon, uterine, or ovarian cancer is common in your family, genetics may play a bigger role than you imagine. Lynch Syndrome is a hereditary condition that increases the risk of these and other cancers. Understanding its genetic basis is the first step toward prevention and detection.
Despite its prevalence, Lynch Syndrome continues to be underdiagnosed due to a lack of awareness and the often subtle nature of its symptoms. Many people may not realize they are carriers of the genetic mutation until they themselves or a family member are diagnosed with cancer. This underscores the importance of genetic counseling and testing for people at risk, as well as proactive surveillance to mitigate the risks associated with this condition. By understanding the complexities of Lynch Syndrome, patients and healthcare professionals can work together to implement effective cancer prevention and early intervention strategies.
The genetic basis of Lynch Syndrome: Mutations in DNA repair genes
The genetic basis of Lynch Syndrome lies in mutations in one of several mismatch repair (MMR) genes. These genes include MLH1, MSH2, MSH6, PMS2, and EPCAM. The primary function of these genes is to correct errors that occur during DNA replication, a process essential for maintaining genetic stability. A genetic mutation in any of these genes can compromise DNA repair, leading to an accumulation of genetic errors. This accumulation significantly increases the likelihood of cancerous tumors forming. This defective repair mechanism underlies Lynch Syndrome and explains the associated cancer risks.
How is Lynch Syndrome inherited?
In people with Lynch Syndrome, the inheritance pattern is autosomal dominant. This means that a single copy of the mutated gene, inherited from either parent, is enough to increase the risk of cancer.
Therefore, if one parent carries a Lynch Syndrome mutation, each child has a 50% chance of inheriting it. It is crucial to remember that having the mutation does not guarantee that you will develop cancer, but it does significantly increase the risk, making proactive measures essential.
What cancer risks are associated with Lynch Syndrome?
People with this syndrome have a significantly higher risk of developing several types of cancer at a younger age than the general population. Colorectal cancer is the most common, but not the only one. Lynch Syndrome also drastically increases the likelihood of developing endometrial cancer and other tumors, such as ovarian, gastric, and urinary tract cancers, among others.
Colorectal Cancer
Colorectal cancer is the type of cancer most commonly associated with Lynch Syndrome. People with this genetic condition have a significantly higher risk and often develop the disease at a younger age compared to the general population.
Endometrial Cancer and Other Tumors
In addition to colorectal cancer, Lynch Syndrome significantly increases the risk of other types of tumors. One of the most important is endometrial cancer, which affects the lining of the uterus.
Lynch Syndrome is also linked to a higher risk of developing ovarian, gastric, small intestine, hepatobiliary tract, urinary tract cancers, and certain types of skin cancer (sebaceous carcinomas). Because of these multiple risks, it is vital to adopt tailored surveillance strategies for each individual.
The Importance of Genetic Testing in Lynch Syndrome
Genetic testing is essential to identify Lynch Syndrome. Generally, these tests involve analyzing a blood or saliva sample to detect mutations in DNA repair genes.
It is crucial to seek genetic counseling both before and after testing. This helps people understand the implications of their results, including the potential impact on their relatives. A positive result indicates that direct family members may also be at risk and should consider getting tested.
Identifying a Lynch Syndrome mutation enables a personalized medical approach, with improved cancer screening protocols and preventive measures. Thanks to this, health outcomes for affected individuals can improve dramatically.
Who should consider genetic testing?
You should consider genetic testing for Lynch Syndrome if you have been diagnosed with colorectal or endometrial cancer (especially if diagnosed before the age of 50). It is also advisable if you have a strong family history of multiple cancers related to the syndrome across several generations.
Other key indicators include having a relative with a confirmed Lynch Syndrome diagnosis, or if your tumor screening results show signs of the disease.
How to prepare for genetic testing
Preparing for genetic testing involves several important steps to ensure you are fully informed. The first step is to seek genetic counseling with a specialist. The counselor will review your personal and family medical history, explain the benefits and limitations of the tests, and discuss what the results could mean for you and your family. This initial consultation is essential to clarify doubts and set realistic expectations.
Before undergoing genetic testing, it is also important to gather as much information as possible about your family’s medical history. This includes data about relatives with cancer, the type of cancer, and the age at diagnosis. A detailed family history helps the genetic counselor determine the likelihood that you have Lynch Syndrome and choose the most appropriate genetic tests. In some cases, the counselor may recommend testing a family member already diagnosed with cancer before testing unaffected relatives.
What do the test results mean?
The results of genetic testing for Lynch Syndrome can be of three types:
– Positive: A genetic variant (pathogenic or likely pathogenic) is found that increases the risk of cancer. This means you have a higher risk of certain cancers and require greater surveillance and preventive measures.
– Negative: No known variant (pathogenic or likely pathogenic) related to the syndrome is found. Generally, this means you do not have a genetic variant associated with Lynch Syndrome, but it is important to keep in mind the limitations of current scientific knowledge and technology.
– Variant of Uncertain Significance (VUS): A genetic variant is found, but there is not enough information yet to determine whether it increases cancer risk.
Prevention and Surveillance
Understanding Lynch Syndrome and its implications is the first step toward taking control of your health. Knowledge about its genetic basis, the associated cancer risks, and the importance of genetic testing is key to making informed decisions and managing the condition proactively. Early detection and regular surveillance are fundamental to mitigating risks and improving health outcomes. That is why counseling and genetic testing are vital to identifying people at risk and designing personalized care plans that can save lives.
Knowing the risks is the first step toward appropriate and personalized medical surveillance.
People who test positive for Lynch Syndrome may undergo colonoscopies more frequently and at a younger age to detect and remove precancerous polyps. For women, regular screening for endometrial and ovarian cancer is also recommended, along with preventive surgeries if they choose. These proactive measures allow early detection and treatment of cancers, significantly improving prognosis and quality of life.
Learning about Lynch Syndrome is important, but the essential step is to move forward. If your family has a history of cancer, a genetic test can help you gain clarity and peace of mind.
At Genosalut, we accompany you with personalized counseling and tests tailored to your needs. Learn more about our genetic testing here.