What is food intolerance?
Food intolerance, also known as non-IgE-mediated food hypersensitivity or non-allergic food hypersensitivity, occurs when a person has difficulty digesting certain foods.
Differences between food intolerance and food allergy
Food intolerances are sometimes confused or mislabelled as food allergies, but they are different phenomena.
● Food allergies trigger strong immune system responses that affect numerous organs in the body. In general, they have a variety of symptoms, although in some cases, an allergic reaction to food can be severe or life-threatening.
● In contrast, symptoms of food intolerance are generally less severe and are often limited to the digestive problems mentioned above.
What are the symptoms of food intolerances?
The most common symptoms of food intolerance are those related to digestive discomfort:
● Diarrhoea
● Bloating
● Flatulence
● Heartburn
● Abdominal cramps
Other symptoms that may appear are:
● Skin rashes
● Dizziness
● Headaches
● General fatigue
● Weight loss
● Growth problems in children
These symptoms may appear shortly after eating the food in question, but sometimes also hours later. As a rule, the symptoms are stronger or weaker depending on the amount of the food consumed.

What are the causes?
Possible causes include:
● Lack or malfunction of certain enzymes to process or utilise food components. For example lactose intolerance.
● Malfunctioning or low amounts of the transporter for absorption of the nutrient (malabsorption).
● Damage to the wall of the small intestine that allows too many harmful substances to enter the bloodstream. In the latter case, experts believe this is due to multiple factors including: today’s diet rich in highly processed foods, stress and harmful environmental influences. For this reason, the number of people with intolerance has continued to rise in recent years.
● Sensitivity to food additives. Such as sulphites, sulphur derivatives which are used as food preservatives and are present in almost all wines, beer, cider, and various foods.
● Recurrent stress or psychological factors.
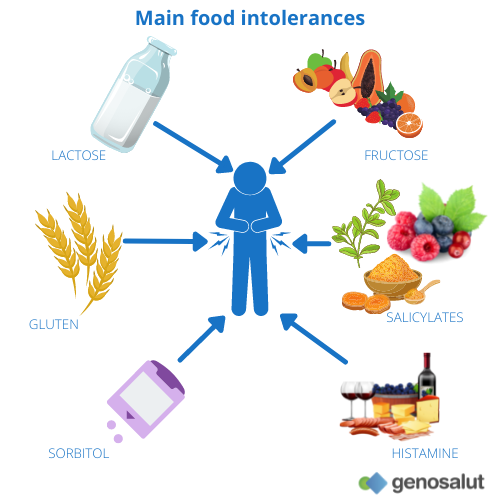
What are the most common food intolerances?
The most common food intolerances are: gluten intolerance or celiac disease, lactose intolerance due to lactase deficiency, histamine intolerance due to diamine oxidase deficiency, fructose intolerance due to glut-5 transporter overload, hereditary fructose intolerance (very rare hereditary enzyme deficiency), lectin intolerance (in wheat, soy and solanaceae), sorbitol intolerance, wheat sensitivity and salicylate intolerance.
Lactose intolerance
For lactose to be used, it has to be broken down in the small intestine by the enzyme lactase. If too little of this enzyme is produced or if it does not function properly, less lactose is metabolised. That is, it is not separated into its two components glucose and galactose. As a result, large amounts of lactose enter the large intestine and are metabolised there by the resident bacteria. The fermentation process causes gas and thus flatulence and unpleasant cramps. It also causes more water to flow into the large intestine, leading to diarrhoea. The formation of lactic acid and acetic acid during fermentation by the bacteria accelerates the movement of the intestines.
What do your genetics say?
The MCM6 gene is primarily responsible for the persistence or non-persistence of lactase activity in adults. This gene contains two of the regulatory regions of LCT, the gene that encodes the lactase protein, located in two of the introns of MCM6. Mutations in these regions are associated with lactose tolerance in adult life. With our nutrigenetic test we analysed the rs182549 variant. It has been shown that people with the CC genotype are genetically predisposed to the development of lactose intolerance. The presence of the C allele in homozygosis reduces lactase enzyme activity. If your genotype is CT or TT, you have a lower risk of lactose intolerance.
What dietary strategy can I use?
You can minimise the incidence and severity of symptoms by reducing lactose intake, seeking alternative sources of nutrients to maintain the necessary energy, calcium and protein intake. The best substitute is lactose-free animal-based dairy or vegetable drinks (soy, oat, rice, hazelnut, almond, etc.), as the bioavailability of calcium in these products is higher. Many lactose intolerant people can ingest small amounts of lactose without symptoms, especially if consumed with other foods. One strategy to improve lactose tolerance is to spread lactose intake in small portions throughout the day. As lactose is found in the aqueous phase of milk, butter does not contain lactose and cured cheeses and natural yoghurts provide very little lactose and are therefore better tolerated.
Fructose intolerance
Fructose is found naturally in fruit and gives it its sweetness. In the case of lactose intolerance, the protein responsible for transporting it from the intestine into the bloodstream malfunctions.
Simultaneous intake of sugar alcohols such as sorbitol, which are found, for example, in diet, light and “sugar-free” products such as candy and chewing gum, further worsens fructose tolerance, so that complaints may increase.
Coeliac disease
What do your genetics say?
After narcolepsy, coeliac disease is the disease most closely associated with HLA, Major Histocompatibility Complex (MHC) Class II. All coeliac patients (100%) carry one of the HLA-DQ2 or DQ8 haplotypes. Only these HLA molecules can carry gliadin antigen fragments. Carriers of these HLA predisposition alleles have a 40-fold increased risk of developing coeliac disease. Furthermore, these gliadin-presenting HLA alleles are an almost mandatory prerequisite for the development of coeliac disease, and it is almost impossible to develop coeliac disease if you do not carry one of these HLA alleles.
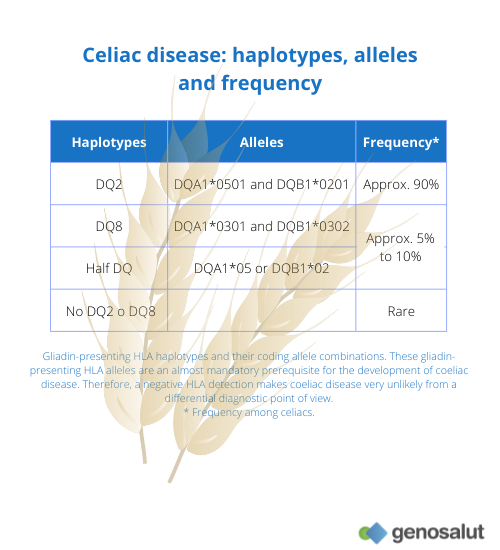
In most of the populations studied, 90-95% of patients carry the HLA-DQ2 heterodimer, encoded by the DQA1*05 and DQB1*02 alleles in cis position (more common in central and northern Europe) or in trans position (more common in Mediterranean countries). The risk of an individual with the DQA1*05:01-DQB1*02:01 heterodimer (DQ2 haplotype) to suffer from the disease is 50 times higher than that of the average population, but its presence does not predict the development of the disease, as it also appears in a quarter of the general healthy population. The remaining patients (5-10%) usually carry the DQA1*03 and DQB1*03:02 heterodimer (DQ8 haplotype) or carry one of the DQ2 haplotype alleles separately (DQA1*05 or DQB1*02). The presence of the DQA1*03 allele in isolation (i.e. in the absence of the DQB1*03:02 allele) does not imply a risk of developing coeliac disease.
What dietary strategy can I apply?
In the case of the development of coeliac disease, the general concept you can follow is: eat gluten-free, healthy and balanced meals, avoiding cross-contamination and unperceived ingestion of gluten. Small amounts of gluten are able to keep the inflammatory process active. Foods suitable for coeliacs should not contain concentrations of gluten higher than 20 ppm. There are food products developed for coeliacs that certify concentrations below 10 ppm. A healthy diet based on natural products and rich in calcium is recommended to avoid cross-contamination. Gluten is an elastic protein that provides structure in many processed food products.
Alcohol hypersensitivity
Alcohol intolerance is caused by a genetic disorder that prevents the body from processing alcohol efficiently.
Alcohol intolerance can cause uncomfortable reactions immediately after drinking alcohol, including:
● Facial redness (flushing).
● Reddened, itchy skin bumps (hives)
● Worsening of pre-existing asthma
● Nasal congestion or runny nose
● Low blood pressure
● Nausea and vomiting
● Diarrhoea
What do your genetics say?
Alcohol intolerance occurs when your body does not have the right enzymes to break down (metabolise) the toxins in alcohol. Among these enzymes is aldehyde dehydrogenase, encoded by the ALDH gene. For the ALDH2 gene, a variant associated with alcohol hypersensitivity has been discovered. This is the rs671 variant. If your genotype is AA or AG, you have a genetic predisposition to develop episodes of alcohol hypersensitivity in response to alcohol intake. The A allele codes for a defective form of the enzyme alcohol dehydrogenase. This causes alcohol to be inefficiently metabolised and accumulate in the blood, causing the dreaded hangover, which can manifest with headache, dizziness, nausea, fatigue, as well as sensitivity to light and sound. If your genotype is GG, you have a lower genetic predisposition to develop these hypersensitivity episodes in response to alcohol consumption.
What dietary strategy can I use?
Although there are other factors that influence tolerance to alcohol consumption, such as gender, body mass and age, avoiding alcohol consumption is the only way to avoid experiencing the adverse effects associated with this type of intolerance.
What can be done in case of food intolerance?
If you have the impression that you do not tolerate certain foods, you can keep a diary of what you eat each day. There you can write down what you eat and when the discomfort occurs. This may give you some initial clues. However, for a definitive diagnosis, you should consult a specialist.
There is no cure for food intolerances and the best treatment is to avoid these foods as much as possible or to eat only what you can tolerate.
Is it possible to test for food intolerance?
Yes, there are different types of tests to determine the presence or predisposition to a food intolerance.
Exhaled hydrogen test: due to incomplete digestion and absorption of lactose and fructose, hydrogen (H2) is produced by the fermentation process of bacteria. This gas can be detected by breath analysis.
In the case of coeliac disease, diagnosis can be complex and includes serology to test for coeliac-related antibodies (mainly anti-transglutaminase antibodies, ATG) and testing for the genetic markers DQ2 and DQ8.
For other types of food intolerances there is no conclusive evidence at this stage.
In general, the causes of gastrointestinal complaints are manifold, both harmless and severe. Food intolerances are not always to blame. Therefore, anyone with severe, persistent or recurrent discomfort should be examined by a doctor.
At Genosalut we have genetic tests to estimate the risk of suffering from coeliac disease, lactose intolerance and fructose intolerance by means of a saliva or blood sample.
If you like our blog, subscribe to our newsletter


