Genetic testing for breast cancer
Genetic testing to determine if you have any mutations associated with an increased risk of breast cancer.
Price
From 180€ (includes genetic counselling)
Time to result
From 2 weeks, depending on the test
Genetic test for breast cancer - Know your risk
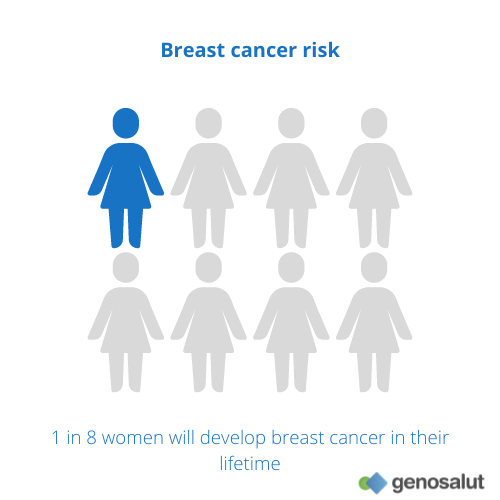
Approximately one in eight women will develop breast cancer in her lifetime. Between five and ten percent of these cases are hereditary breast cancer. Thanks to our genetic tests we can determine whether a person has a higher risk of suffering from this disease and we can also establish whether the cases of breast cancer in a family have a hereditary cause. A genetic test is indicated if:
- You suffer or have suffered from breast cancer. In this case, genetic diagnosis can clarify your risk of developing a second tumour, as well as the possible risks of other family members.
- If you have a family history of breast cancer or particularly early breast cancer. In this case genetic testing of your family, preferably of an affected member, can assess your personal risk.
Genetic testing for breast cancer
At Genosalut we have more than ten years of experience in carrying out genetic tests for cancer. We attend patients who come directly to our clinic and we also work with a network of specialist doctors who trust us to carry out these tests on their patients.
In the drop-down menu you will find information about the different genetic tests for colorectal cancer that we offer in our laboratory:
Familial mutation
Study of a clinically relevant genetic variant associated with hereditary breast cancer present in other previously diagnosed family members.
Panels
Analysis by massive sequencing of the following genes associated with an increased risk of developing breast cancer: BRCA1, BRCA2, MLH1, MSH2, MSH6, PMS2, EPCAM, TP53, PTEN, STK11, CDH11, PALB, CHEK2, ATM, NBN, BARD1, BRIP1, RAD51C and RAD51D. Includes fragment analysis of BRCA1, BRCA2 and EPCAM genes.
Exome
Thanks to the sequencing of all genes using next generation sequencing (NGS) techniques, we can determine the presence of mutations associated with hereditary breast cancer.
Genome
Thanks to the sequencing of all coding (gene) and non-coding regions using next generation sequencing (NGS) techniques, we can determine the presence of mutations associated with hereditary breast cancer.
Our value proposal
Experience
At Genosalut, we have more than 10 years of experience in counselling people with conditions where a genetic cause has been identified or is thought to be possible.
Proximity
We are a close laboratory, we respond personally and we take the time to explain the report in detail to doctors and patients.
Professional interpretation of results
Because of our knowledge and experience, we are able to accurately interpret genetic results and offer professional advice.
Reference in the field
We are the point of contact for patients, doctors and clinics in all areas of human genetic diagnostics and prevention.
Breast cancer risk with BRCA1 and BRCA2 mutations
BRCA1 and BRCA2 were the first two genes to be associated with familial breast cancer. These two genes produce proteins that repair DNA damage. Each person inherits two copies of each of these genes: one from the mother and one from the father.
People who inherit a BRCA1 or BRCA2 variant mutation have an increased risk of several types of cancer, particularly breast and ovarian cancer. They also tend to develop cancer at a younger age than those who do not.
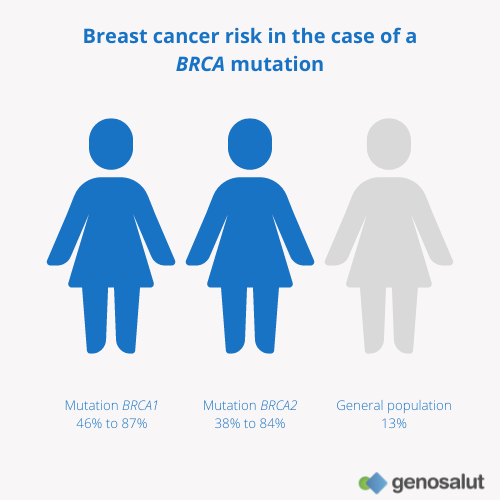
Approximately 13% of women in the general population will develop breast cancer at some point in their lives. For women with a mutation in the BRCA1 gene, between 46% and 85% of them will develop the disease before the age of 80. For women with a BRCA2 mutation, the risk is between 38% and 84%. The risk for any one woman depends on a number of factors whose characteristics are not yet fully understood.
Prevention and peace of mind with the genetic tests of Genosalut
Together with your doctor you can determine strategies for early detection
If you are found to have a known mutation associated with an increased risk of breast cancer, you can participate in intensive screening programmes for the early detection of these tumours, which may include earlier and more frequent mammograms. The earlier a tumour is detected, the better the chances of a cure.
You will know if you can pass on the risk to your offspring
Conversely, if you do not carry the mutation in your family, you know that your risk of breast cancer is the same as the general population. Your offspring, therefore, will not have an increased risk either.
How can I request a genetic test for breast cancer?
Request an appointment
Contact us through the form, by e-mail or by telephone to make an appointment with us.
Ask your physician
You can also consult your doctor for information on the possibilities of genetic testing.
We analyse the probe
In our genetic diagnostics laboratory we analyse the sample with the latest technology.
We write a report
We provide a detailed description of the results and, if necessary, genetic counselling.
FAQs
What is breast cancer?
The term “breast cancer” describes a malignant tumour that develops from breast cells. There are different types of breast cancer, depending on which cells in the breast become cancerous. In most cases, breast cancer starts in the cells of the milk-producing glands, or in the cells of the ducts that drain milk to the nipple. Less commonly, breast cancer can develop in the stromal tissues, which include the fatty and fibrous connective tissues of the breast.
Over time, cancer cells can invade nearby healthy breast tissue and make their way out of the breast through blood vessels and lymphatic vessels. If the cancer cells spread to other parts of the body, metastasis occurs.
While it is true that breast cancer mainly affects women, men, too, can very rarely (about 1%) develop the disease.
What is the risk of breast cancer?
Regarding the incidence of breast cancer, statistics indicate that 1 in 8 women may develop breast cancer at some point in their lives. This absolute risk should be taken as a starting point, since each woman’s individual risk may be higher or lower, depending on non-controllable factors such as gender, age (most cases are detected in women over 50), family history or reproductive history. It also depends on controllable factors such as weight, physical activity or alcohol consumption.
What causes breast cancer? Sporadic and hereditary
Breast cancer is always caused by a genetic abnormality (an “error” in the genetic material). Most of the time, 85-90% of the time, these genetic abnormalities occur sporadically, as a result of the natural ageing process. However, the remaining 5-10% are due to a genetic abnormality inherited from the father or mother.
What can be done to prevent breast cancer?
Along with a healthy lifestyle, gynaecological screening is an essential tool for the prevention and early detection of breast cancer. When breast cancer is detected at an early stage, there is a good chance of recovery.
In the case of a family history, it may also be advisable to have a genetic test to determine if there is an increased risk. In case of a positive result, this will help to determine further preventive strategies.
BRCA genes and other genes associated with hereditary breast cancer risk
Historically, the first two genes to be associated with familial breast cancer were BRCA1 and BRCA2. We now know that those who inherit mutations in these genes have an increased risk of developing breast cancer and ovarian cancer compared to the general population. For example, the risk of breast cancer is much higher in women who have inherited mutations in BRCA1 or BRCA2. For women with a BRCA1 mutation, the risk of developing breast cancer at age 80 is 72%. This means that out of every 100 women who have this mutation, about 72 can expect to develop breast cancer if they live to age 80. For women with a BRCA2 mutation, the risk is slightly lower, at 69%.
BRCA genes are not the only cancer risk genes. Various studies carried out in recent years have identified other genes associated with an increased risk of breast cancer. These genes include RAD51C, RAD51D, CHEK2, ATM, BRIP1, PALB2, TP53 and CDH1. Recently, the BARD1 gene has also been added as a moderate risk gene for breast cancer. In most cases, the results obtained from the analysis of these genes allow a detailed and informative genetic counselling and a specific recommendation on the clinical procedure.
When family history suggests the presence of a heritable mutation, or if a close relative has a mutation in one of the risk genes, predictive genetic testing can be offered.
What is the genetic test for breast cancer used for?
Genetic testing for breast cancer is indicated in patients with a family history suggestive of a familial mutation.
What results can I get from a genetic test?
Positive result matching the mutation found in the family
If you have tested positive and have been found to have the known familial mutation that is or was responsible for the development of breast cancer in your family, then you have a significantly higher risk of developing the disease in your lifetime than the rest of the population. It does not imply that you have or will develop the disease, but it does imply that you should intensify surveillance and follow preventive guidelines. In addition, there may be an increased risk of cancer for their offspring.
Positive result in a family in which the causal mutation is not known to exist
In the case of a positive result in a patient for whom no family member with the disease has been or can be tested, it can be assumed that the same mutation also caused the disease in family members who developed breast cancer. In other words, this person also has a higher risk of developing cancer.
Negative result in a family with known causal mutation
If you have a negative result, this means that the known familial mutation responsible for the development of breast cancer in the family is not detected in the patient or that there may be a mutation in a gene that has not yet been associated with breast cancer. This means that you do not have an increased risk of developing breast cancer. Therefore, you have the same risk as the general population (approximately 4%) of developing breast cancer in your lifetime.
Negative result in a family with no known causal mutation
If no known mutation has been found in any family member despite there being some people affected by breast cancer, it may be that another gene is responsible for the development of the cancer and/or that the cancers in your family are not due to an inherited predisposition.
Finally, the result of the genetic test may indicate the presence of a genetic variant that doctors do not have enough information about to be able to assess correctly (variant of uncertain (unknown) significance, VUS). In these situations, the benefit to the patient cannot always be defined.
In which cases is a genetic test for breast cancer indicated?
In order to decide whether a genetic test is advisable, it is ideally important to compile a family tree over 3 generations. By analysing this tree, it can be determined whether there is an increased risk of disease for breast and ovarian cancer and a genetic test can be recommended. As a general rule, it is recommended if at least one of the following criteria is met:
- 3 women with breast cancer, regardless of age
- 2 women with breast cancer, one of whom was diagnosed before her 51st birthday
- 1 woman with breast cancer and 1 woman with ovarian cancer
- 1 woman with breast and ovarian cancer
- 2 women with ovarian cancer
- 1 woman with bilateral breast cancer, first breast cancer before 51 years of age
- 1 woman with breast cancer before the age of 36 years
- 1 male with breast cancer and 1 female with breast or ovarian cancer
If you have or have already had cancer, it is advisable to undergo the study when:
- You have ovarian cancer
- You have or have had triple negative breast cancer before the age of 50 (absence of both hormone receptors and the HER2 receptor)
- In case of therapeutic relevance (e.g. use of PARP inhibitors in women with HER2-negative advanced/metastatic breast cancer and BRCA1/2 mutation)
Genetic counselling for the genetic screening of breast cancer
The decision about whether or not to have a genetic test to establish the risk of breast cancer is a personal one and should always be made after genetic counselling. This counselling should try to answer any questions about:
- What it means to do the test
- How the patient may feel while waiting for the results to come back
- What kind of actions can be considered after the results have been obtained
What are the benefits of genetic testing for breast cancer?
Genetic diagnosis is an essential preventive tool. If a mutation in one of the genes is detected through genetic diagnosis, the risk of developing cancer increases considerably. It is therefore vital that people carrying the mutation undergo different preventive diagnostic methods on a regular basis.
Accurate and regular follow-up is essential to reduce the incidence of cancer and radically reduce the associated mortality.
Who covers the costs of genetic counselling and diagnosis of breast cancer?
There are private insurance policies that cover preventive genetic analysis in first-degree relatives of affected persons with a detected familial mutation.
However, there are private insurances that do not cover the costs and are therefore paid by the patient.
Request an appointment with us
Opening hours
Monday to Friday from 9.00 am to 1.00 pm
+34 616 59 01 65
info@genosalut.com
Camí dels Reis, 308 (Clínica Palma Planas)
Contact form
Reasons for trusting Genosalut
First genetic diagnosis laboratory in the Balearic Islands
Professionals with experience in medical genetics
Detailed report of the results
Personalised attention for each patient
Wide range of genetic tests
Cutting-edge technology