Genetic testing for colorectal cancer
Genetic testing to determine if you have any mutations associated with an increased risk of colorectal cancer.
Price
From 180€ (includes genetic counselling)
Time to result
From 2 weeks, depending on the test
Genetic test for colon cancer - Know your risk
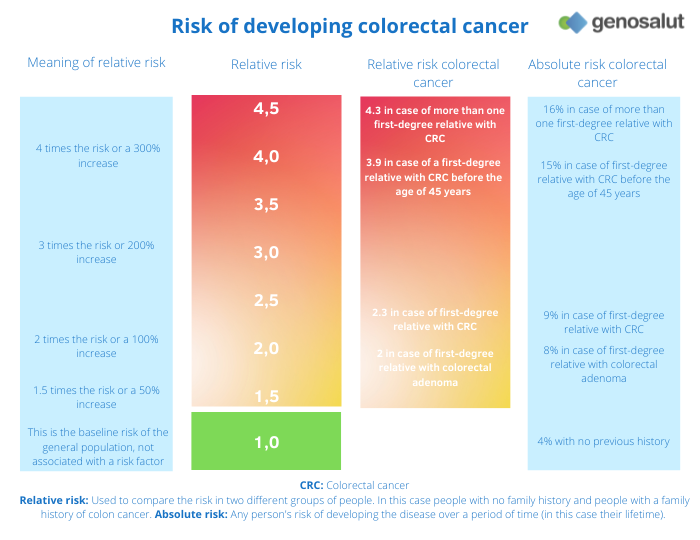
The lifetime risk of colorectal cancer in the general population is approximately 1 in 23 (4.3%) for men and 1 in 25 (4.0%) for women. However, this risk can increase by a factor of 4 if there is a family history of colon or rectal cancer (relative risk indicated in the table).
If any of the following statements apply in your family, it may indicate a family history of colorectal cancer and further evaluation is recommended:
- One person in the family under the age of 60 with colorectal cancer.
- Two people in the family with colorectal cancer.
- One person with small bowel cancer.
Genetic testing for colorectal cancer
At Genosalut we have more than ten years of experience in carrying out genetic tests for cancer. We attend patients who come directly to our clinic and we also work with a network of specialist doctors who trust us to carry out these tests on their patients.
In the drop-down menu you will find information about the different genetic tests for colorectal cancer that we offer in our laboratory:
Familial mutation
Study of a clinically relevant genetic variant associated with hereditary colorectal cancer present in other previously diagnosed family members.
Methylation of the SEPT9 gene
Early detection of colon cancer by determining the methylation status of the SEPT9 gene.
Panels
Study of variants of the APC, AXIN2, BMPR1A, CDH1, CHEK2, EPCAM, GALNT12, GREM1, MLH1, MSH2, MSH3, MSH6, MUTYH, NTHL1, PMS2, POLD1, POLE, PTEN, RNF43, RPS20, SMAD4, STK11 and TP53 genes related to HNPCC. Includes fragment analysis of APC, EPCAM, MLH1, MSH2, MSH6 and PMS2 genes.
Exome
Thanks to the sequencing of all genes using next generation sequencing (NGS) techniques, we can determine the presence of mutations associated with hereditary colorectal cancer.
Genome
Thanks to the sequencing of all coding (gene) and non-coding regions using next generation sequencing (NGS) techniques, we can determine the presence of mutations associated with hereditary colorectal cancer.
Our value proposal
Experience
At Genosalut, we have more than 10 years of experience in counselling people with conditions where a genetic cause has been identified or is thought to be possible.
Proximity
We are a close laboratory, we respond personally and we take the time to explain the report in detail to doctors and patients.
Professional interpretation of results
Because of our knowledge and experience, we are able to accurately interpret genetic results and offer professional advice.
Reference in the field
We are the point of contact for patients, doctors and clinics in all areas of human genetic diagnostics and prevention.
Hereditary and familial colorectal cancer
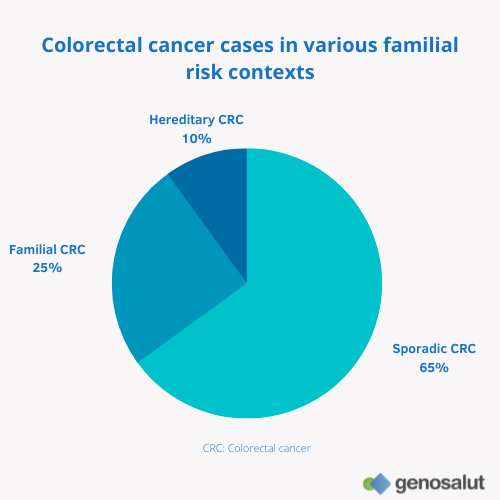
Up to 35% of colorectal cancer cases are associated with an increased familial risk. Out of all cases, 10% of patients have hereditary colorectal cancer (associated mutation known) and 25% of patients have familial colorectal cancer (mutation and/or other associated factors unknown).
These hereditary syndromes are characterised by the presence of mutations in some genes, mainly those responsible for controlling cell division and repairing our DNA. These mutations can be transmitted from generation to generation.
With regard to colorectal cancer, the two most common syndromes are familial adenomatous polyposis (FAP) and Lynch syndrome (also known as hereditary non-polyposis colon cancer, HNPCC). Other types of hereditary colorectal cancer include juvenile polyposis syndrome, serrated polyposis syndrome, Cowden syndrome, MUTYH-associated polyposis syndrome and Peutz-Jeghers syndrome.
Prevention and peace of mind with the genetic tests of Genosalut
Together with your doctor you can determine strategies for early detection
If you are found to have a known mutation associated with an increased risk of colorectal cancer, you can participate in intensive screening programmes for early detection of these tumours, which may include earlier and more frequent abdominal ultrasounds, colonoscopies and rectoscopies. The earlier a tumour is detected, the better the chances of cure.
You will know if you can pass on the risk to your offspring
Conversely, if you do not carry the mutation in your family, you know that your risk of colorectal cancer is the same as the general population. Your offspring, therefore, will not have an increased risk either.
How can I request a genetic test for colorectal cancer?
Request an appointment
Contact us through the form, by e-mail or by telephone to make an appointment with us.
Ask your physician
You can also consult your doctor for information on the possibilities of genetic testing.
We analyse the probe
In our genetic diagnostics laboratory we analyse the sample with the latest technology.
We write a report
We provide a detailed description of the results and, if necessary, genetic counselling.
FAQs
What is colorectal cancer?
Colon or colorectal cancer is cancer that originates in the colon or rectum.
The colon and rectum are part of the digestive tract, the final section of our intestine. The colon is about 1.5 metres long and runs in an inverted U-shape through the abdominal cavity. Its function is to absorb water and minerals from the faeces. Right at the end of the colon is the rectum. The rectum is a little less than an inch long and is the end of the passage of our faeces, where they are stored until the time of defecation.
What is the risk of colorectal cancer?
The incidence of colon cancer in Spain is approximately 15%. This means that 15% of all cancers diagnosed in a year in Spain are colon cancer. Overall, the lifetime risk of developing colon cancer is approximately 4%. In terms of mortality, colon cancer is the second leading cause of cancer-related death in men, after lung cancer. Similarly, colorectal cancer in women is also second only to breast cancer.
What are the main causes of colon cancer?
As with the other cancers, changes in a cell’s genetic material or mutations are the cause.
In up to 10% of cases, these mutations may be inherited (hereditary colorectal cancer), in about 25% there is a familial association with no known causal mutation (familial colorectal cancer) and in the remaining 65% of cases the mutations occur throughout life (sporadic colorectal cancer). They can be caused by harmful substances, but can also occur accidentally during cell division. Normally, cells have repair systems to eliminate defects that originate in genes, but these mechanisms are more likely to fail as we age.
In most patients, intestinal tumours originate in the glandular cells of the mucosa lining the inside of the intestine (adenocarcinomas). These cells begin to proliferate and generate polyps or clusters of non-cancerous (benign) cells, which slowly develop into malignant cancer cells.
Although in most cases of colorectal cancer it is not possible to find a specific cause, we do know some of the risk factors that are associated with the development of colon cancer.
- Age over 50 years
- Inflammatory bowel diseases such as ulcerative colitis or Crohn’s disease
- A diet high in fat and low in fibre
- Obesity
- Smoking
- Alcohol
- A family history of colon cancer is also a risk factor. The more members of the same family who have had colon cancer (especially first-degree relatives such as parents, siblings or children), the greater the likelihood of developing it.
What can be done to prevent colon cancer?
It is advisable to follow a healthy lifestyle:
- Eat vegetables, fruit and whole grains and try to avoid red meat (beef, pork or lamb) and processed meats (sausages and some cold meats), which have been linked to an increased risk of colorectal cancer.
- Take regular physical exercise.
- Control your weight.
- Do not smoke.
- Do not drink alcohol.
In addition, it is important to participate in screening tests, especially for those at increased risk. These tests allow cancer to be detected before signs and symptoms appear and treatments can be started when they are most likely to be successful.
In the case of a family history, it is also advisable to have a genetic test to determine if there is an increased risk. In case of a positive result, this will help determine further preventive strategies to be taken.
What is Lynch Syndrome or hereditary non-polyposis colon cancer (HNPCC)?
Lynch syndrome is an inherited form of predisposition to some types of cancer, mainly colon cancer and endometrial or uterine cancer in women.
One of the characteristics of Lynch syndrome is the early onset (between 40 and 45 years of age) of colon cancer.
What is the risk of inheriting or transmitting Lynch syndrome?
When a person is diagnosed with Lynch syndrome, their offspring have a 50% chance of inheriting the genetic mutation that causes the syndrome.
How do I know if I have Lynch syndrome?
First of all, personal and family history should be established, especially colon and endometrial cancer at an early age. If this history raises the suspicion of Lynch syndrome, genetic studies and other corresponding diagnostic tests can be performed.
Why can certain genetic changes cause Lynch syndrome?
Almost all tissues in the body are renewed by cell division. During this process, a copy of the genetic material is created and passed on to daughter cells. Copies of the genetic material are always flawed (just as a photocopy will never be like the original document), but cells have repair systems to correct them. In Lynch syndrome patients, these repair systems are defective, leading to the accumulation of genetic errors and the development of cancer. In the specific case of Lynch syndrome these errors manifest themselves as microsatellite instability.
Which genes are associated with Lynch syndrome?
DNA repair systems are defective because some of the ‘repair genes’ (those encoding the proteins that carry out the actual repair) are mutated. So far, mutations in the following genes have been associated with Lynch syndrome: MLH1, MSH2, MSH6, PMS2 and EPCAM. Genetic testing for Lynch syndrome will detect whether or not a patient suspected of having Lynch syndrome (based on family history) has any of the mutations associated with this disease.
What is the risk of developing cancer if diagnosed with Lynch syndrome?
Patients with mutations in the MLH1, MSH2, MSH6, PMS2 and EPCAM genes (on average for all mutations) have a lifetime chance of developing cancer of 10% to 80% (depending on the genetic mutation causing the syndrome) compared to 4% in the general population. The lifetime prevalence of colorectal cancer is 30-75%. Women with one of these mutations develop endometrial cancer at a rate of 40-50%. The risk of stomach, ovarian, pancreatic, urothelial, biliary tract or small bowel cancer and glioblastomas is also slightly increased. Sebaceous gland adenomas and keratoacanthomas may also occur.
What is familial adenomatous polyposis (FAP)?
Familial adenomatous polyposis is a hereditary type of colorectal cancer caused by mutations in the APC gene.
It is characterised by the appearance at a very young age (from 10 years old) of a large number of initially benign polyps, mainly in the colon area. If left untreated, one or more of these polyps will develop into colon cancer (colorectal carcinoma) in an unpredictable time. Therefore, early detection and treatment of these polyps is crucial.
What are the types of PAF?
- Classic FAP: typically characterised by more than 100 colorectal polyps.
- Attenuated FAP (AFAP): characterised by a later age of onset and usually a much smaller number of polyps (< 100) in the colon. Despite the milder course, the lifetime risk of colon cancer is similar to that of classic FAP.
- Gardner syndrome is a variant of FAP. People with this syndrome have multiple adenomatous colon polyps, but also other tumours outside the gastrointestinal organs (epidermoid cysts, fibromas, desmoid tumours, osteomas).
- Turcot syndrome is considered a variant of FAP or Lynch syndrome. People with this syndrome have many adenomatous colon polyps, an increased risk of colorectal cancer and an increased risk of brain tumours (glioblastoma and medulloblastoma).
What is the risk of inheriting or transmitting familial adenomatous polyposis?
When a person is diagnosed with FAP, their offspring have an approximately 50% chance of inheriting the genetic mutation that causes the syndrome.
Which genes are associated with familial adenomatous polyposis?
As mentioned above, genetic alterations or mutations in the APC gene are associated with the different types of FAP. In most cases it is an inherited mutation, although in 1 in 3 patients it is a de novo germline mutation in the APC gene.
Genetic testing for familial adenomatous polyposis will detect whether or not a patient suspected of having the syndrome (based on family history) has any of the mutations associated with this disease.
What other cancers are associated with PAF?
People with FAP are also more likely to have cancers in other organs: stomach, small intestine, pancreas and bile ducts. There is also an increased risk of hepatoblastoma, desmoid tumour/desmoid fibromatosis, papillary thyroid cancer, and a rare type of brain tumour called medulloblastoma.
What is the purpose of genetic testing for colorectal cancer and what are the benefits?
Genetic diagnosis is an essential preventive tool for people with a family history suggestive of a familial mutation.
If a mutation is detected in one of the genes through genetic diagnosis, the risk of developing cancer increases considerably. It is therefore important that people carrying a mutation undergo different diagnostic methods to reduce the incidence of cancer and reduce the mortality associated with the syndrome.
What results can I get from a genetic test?
Positive result matching the mutation found in the family
If you have tested positive and have been found to have the known familial mutation that is or was responsible for the development of colorectal cancer in your family, then you have a significantly higher risk of developing the disease in your lifetime than the rest of the population. It does not imply that you have or will develop the disease, but it does imply that you should intensify surveillance and follow preventive guidelines. In addition, there may be an increased risk of cancer for their offspring.
Positive result in a family in which the causal mutation is not known to exist
In the case of a positive result in a patient for whom no family member with the disease has been or can be tested, it can be assumed that the same mutation also caused the disease in family members who developed colorectal cancer. In other words, this person also has a higher risk of developing cancer.
Negative result in a family with known causal mutation
If you have a negative result, this means that the known familial mutation responsible for the development of colorectal cancer in the family is not detected in the patient or that there may be a mutation in a gene that has not yet been associated with colorectal cancer. This means that you do not have an increased risk of developing colorectal cancer. Therefore, you have the same risk as the general population (approximately 4%) of developing colorectal cancer in your lifetime.
Negative result in a family with no known causal mutation
If no known mutation has been found in any family member despite there being some people affected by colorectal cancer, it may be that another gene is responsible for the development of the cancer and/or that the cancers in your family are not due to an inherited predisposition.
Finally, the result of the genetic test may indicate the presence of a genetic variant that doctors do not have enough information about to be able to assess correctly (variant of uncertain (unknown) significance, VUS). In these situations, the benefit to the patient cannot always be defined.
In which cases is a genetic test for colorectal cancer indicated?
For Lynch syndrome, one of the following criteria is usually used:
Amsterdam criteria
At least 3 relatives have a cancer related to Lynch syndrome and:
- One is a first-degree relative (parent, sibling or child) of the other 2 relatives.
- At least 2 successive generations are affected.
- At least 1 relative had the cancer when they were younger than 50 years old.
Bethesda criteria:
- The person is younger than 50 years of age when diagnosed with colorectal cancer.
- The person has or has had a second colorectal cancer or another cancer (endometrial, stomach, pancreatic, small bowel, ovarian, kidney, brain, ureter, or bile duct) related to Lynch syndrome.
- The person is under 60 years of age and the cancer has certain features seen in Lynch syndrome when viewed under a microscope.
- The person has a first-degree relative (parent, sibling or child) under the age of 50 who has been diagnosed with colorectal cancer or another cancer related to Lynch syndrome.
- The person has 2 or more first- or second-degree relatives (aunts, uncles, nieces, nephews, or grandparents) who had colorectal cancer or other Lynch syndrome-related cancer at any age.
Genetic counselling for the genetic screening of colorectal cancer
The decision about whether or not to have a genetic test to establish the risk of colorectal cancer is a personal one and should always be made after genetic counselling. This counselling should try to answer any questions about:
- What it means to do the test
- How the patient may feel while waiting for the results to come back
- What kind of actions can be considered after the results have been obtained
Who covers the costs of genetic counselling and diagnosis of colorectal cancer?
There are private insurance policies that cover preventive genetic analysis in first-degree relatives of affected persons with a detected familial mutation.
However, there are private insurances that do not cover the costs and are therefore paid by the patient.
Request an appointment with us
Opening hours
Monday to Friday from 9.00 am to 1.00 pm
+34 616 59 01 65
info@genosalut.com
Camí dels Reis, 308 (Clínica Palma Planas)
Contact form
Reasons for trusting Genosalut
First genetic diagnosis laboratory in the Balearic Islands
Professionals with experience in medical genetics
Detailed report of the results
Personalised attention for each patient
Wide range of genetic tests
Cutting-edge technology
