Test for thrombophilia associated with fertility problems
Tests for the most common types of genetically caused thrombophilia associated with problems in pregnancy.
Price
230€ (includes genetic counselling)
Time to result
2 weeks
How do thrombophilias influence pregnancy?
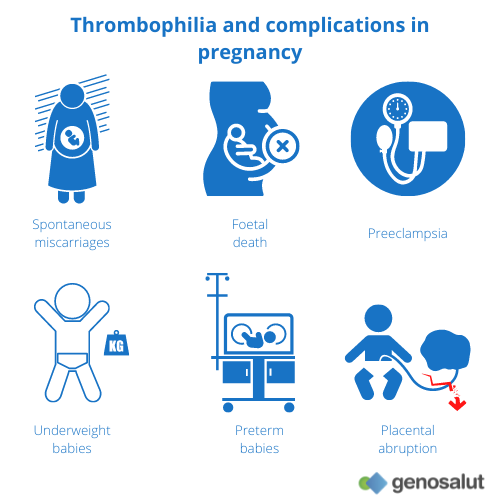
Thrombophilias are a group of blood coagulation disorders, characterised by an increase in the coagulability of the blood and the tendency for thrombi or clots to form. They are multifactorial disorders in which both environmental factors (age, smoking, overweight, etc.) and genetic predisposition may play a role.
Evidence supports an association between certain types of thrombophilia and some specific problems in relation to the infertile couple. These coagulation disorders can hinder embryo implantation, impede normal foetal development and lead to miscarriage.
Congenital (e.g. factor V Leiden mutation) or acquired (antiphospholipid antibodies) tendency to thrombosis can be detected with the help of laboratory tests and thus appropriate measures can be taken in situations of fertility problems and risky pregnancies. For diagnosis, various genetic and coagulation tests are usually carried out.
These tests are especially recommended for pregnant women (or women who wish to become pregnant) who have already had a thrombosis or who have a family history of thrombosis. Repeated miscarriages and pre-eclampsia (gestosis, HELLP syndrome) are also considered indications.
Study of thrombophilia in the context of fertility
At Genosalut we analyse by HRM (high resolution melting) the most frequent mutations associated with cases of hereditary thrombophilia: Factor V Leiden, Factor II (prothrombin), methylenetetrahydrofolate reductase (MTHFR) and Factor XIII.
Factor V Leiden (rs6025 variant)
The presence of Factor V Leiden is the most common of the known inherited pathologies affecting blood clotting and is detected in about a quarter of all patients with thrombosis.
It is a point mutation in the Coagulation Factor V gene (a G>A change at position 1691) that transforms amino acid 506 from arginine to glutamine and causes an alteration in the structure of the protein that prevents its inactivation by active protein C and leads to the formation of venous thrombi.
In the general European population, 0.5% to 5% are heterozygous carriers and 0.05% to 0.5% are homozygous carriers. Heterozygosity for factor V Leiden is associated with a 5 to 10-fold increased risk of venous thrombosis. For homozygous trait carriers, the individual risk of thrombosis increases by 50 to 100 times.
For pregnant women, the presence of this mutation can lead to an increased risk of thrombosis of up to 1:10 (being 1:500 in healthy pregnant women).
Inheritance is autosomal dominant with incomplete penetrance.
Protrombina o Factor II (variante rs1799963)
The second most frequent genetic defect in the coagulation system is the prothrombin (Factor II) gene mutation (present in 6-7% of thrombotic patients). Point mutation in the 3′ non-coding region of the prothrombin gene (G>A change at position 20210) is associated with elevated plasma prothrombin levels and thrombophilia. This prothrombin variant is associated with a 3-5-fold increased risk of thrombosis, as well as an increased risk of adverse pregnancy outcomes including early and recurrent miscarriage.
In pregnant women, the presence of this mutation can lead to an increased risk of thrombosis of up to 1:10 (1:500 in healthy pregnant women).
Inheritance is autosomal recessive.
MTHFR (variants rs180113 and rs 1801131)
Methylenetetrahydrofolate reductase (MTHFR) is another gene that plays an essential role in the arterial and venous vascular system.
The two variants rs1801133 and rs 1801131 have been associated with decreased enzyme activity and increased plasma homocysteine levels.
- The rs1801133 variant involves a C>T change at position 677 that transforms amino acid 222 from alanine to valine. Individuals with the homozygous 677TT variant have no more than 30% of normal enzyme activity, and heterozygotes of the CT genotype have 65% of normal enzyme activity and increased thermolability.
- The rs1801131 variant involves an A>C change at position 1298 that transforms amino acid 429 from glutamine to alanine. Heterozygous (AC) and homozygous (CC) carriers have a reduction in enzyme activity of 15% and 30%, respectively.
These mutations in MTHFR may increase the risk of:
- Cardiovascular disease
- Kidney failure
- Chromosomal abnormalities
- Spontaneous miscarriage
- Other diseases
Inheritance of both variants is autosomal recessive.
Factor XIII (rs5985 variant)
This variant involves a G>T change at position 103 that transforms amino acid 34 from valine to leucine. The less frequent allele (T) is considered protective against thromboembolism.
Our value proposal
Experience
At Genosalut, we have more than 10 years of experience in counselling people with conditions where a genetic cause has been identified or is thought to be possible.
Proximity
We are a close laboratory, we respond personally and we take the time to explain the report in detail to doctors and patients.
Professional interpretation of results
Because of our knowledge and experience, we are able to accurately interpret genetic results and offer professional advice.
Reference in the field
We are the point of contact for patients, doctors and clinics in all areas of human genetic diagnostics and prevention.
When it is recommended to test for thrombophilia
Thrombophilias are not part of the basic infertility work-up. As mentioned above, the association between thrombophilia and fertility problems is evident in certain cases. Therefore, they are very specific tests, which are requested when there is a suspicion that they may be influencing the reproductive history of the couple or woman.
The main cases in which we must rule out or confirm the presence of thrombophilias are the following:
- Two or more miscarriages before the tenth week of pregnancy.
- One or more miscarriages after the tenth week of pregnancy.
- Premature birth before the 34th week of pregnancy.
- Personal history of thromboembolism.
- Implantation failure. Absence of gestation after several transfers, having transferred a total of four or more embryos of good quality.
- History of intrauterine foetal death.
- Family history of repeated miscarriage or thromboembolism.
- Severe or early pre-eclampsia.
- Premature detachment of the placenta (abruptio placentae).
In summary, having had a single miscarriage or a negative transfer, in the absence of the above risk factors, are common circumstances in the general population and do not normally raise suspicion of thrombophilia.
Information from the thrombophilias study
You can find out what causes fertility problems
The detection of a genetic defect associated with thrombophilia may be the cause of fertility problems in women. Knowledge of this result and counselling by our specialists will allow you to know the possibilities of treatment.
You can know the risk of having affected offspring
The detection of a genetic defect associated with thrombophilia implies a risk of having offspring who are also affected by the condition.
How can I request a thrombophilia study?
Request an appointment
Contact us through the form, by e-mail or by telephone to make an appointment with us.
Ask your physician
You can also consult your doctor for information on the possibilities of genetic testing.
We analyse the probe
In our genetic diagnostics laboratory we analyse the sample with the latest technology.
We write a report
We provide a detailed description of the results and, if necessary, genetic counselling.
Frequently asked questions
What are thrombophilias and how are they classified?
Thrombophilias are a group of disorders characterised by the abnormal formation of clots in the blood:
They are classified into two groups:
- Acquired thrombophilias, which occur due to diseases or external agents. These include autoimmune thrombophilias or antiphospholipid syndrome (APS).
- Genetic thrombophilias, which are caused by a defect in a gene related to blood coagulation. These include Factor II and Factor V Leiden mutation, among others.
What external factors predispose to thrombosis?
In most patients with a hereditary predisposition, thrombosis does not occur spontaneously, but is promoted by external risk factors. These factors are very variable and can be, for example: smoking, obesity, lack of exercise, contraceptive pills, pregnancy…
How is thrombophilia diagnosed?
The first step in the diagnosis of thrombophilia is usually a blood test to check the level of coagulation. This is usually followed by a more specific test that includes genetic and/or coagulation testing for the following factors:
- Standard antibody
- Protein Z antibody
- Anti-annexin V antibody
- Factor V Leiden
- Factor VIII
- Factor XIII
- ABO genotype
- Homocysteine
- Factor XII C46T polymorphism
These tests are usually done only when there is an indication for them, such as incidents of thrombosis, family history, recurrent miscarriages, etc.
Why does the risk of thrombosis increase during pregnancy?
During pregnancy a woman’s body undergoes many changes, including changes in blood composition:
- Increased synthesis of clotting factors
- Increased resistance of activated protein C
- Decrease in natural anticoagulants such as protein S
- Increased venous congestion
All these factors lead to the production of blood clots, which can cause thrombosis in the placental vessels and stop the development of the foetus.
Can thrombophilia be treated during pregnancy?
If the diagnosis of thrombophilia is confirmed, it is important that the gynaecologist collaborates with the haematologist to determine the appropriate treatment to enable pregnancy.
The most common treatment is anticoagulants such as aspirin and heparin before and during pregnancy.
Thrombophilia and assisted reproduction
Thrombophilia may be diagnosed in the context of fertility consultations.
If a diagnosis of thrombophilia is confirmed in the woman, aspirin and heparin are usually scheduled during controlled follicular stimulation. This treatment allows a high percentage of women to become pregnant and give birth to a healthy child. However, some women still miscarry even with anticoagulants and are unable to give birth.
Who covers the costs of the genetic test for thrombophilia?
Genetic testing for thrombophilia is covered by some private insurances and sometimes depends on the fulfilment of certain diagnostic criteria. You can come to us with a certificate from your doctor or with your insurance card.
Request an appointment with us
Opening hours
Monday to Friday from 9.00 am to 1.00 pm
+34 616 59 01 65
info@genosalut.com
Camí dels Reis, 308 (Clínica Palma Planas)
Contact form
Reasons for trusting Genosalut
First genetic diagnosis laboratory in the Balearic Islands
Professionals with experience in medical genetics
Detailed report of the results
Personalised attention for each patient
Wide range of genetic tests
Cutting-edge technology
