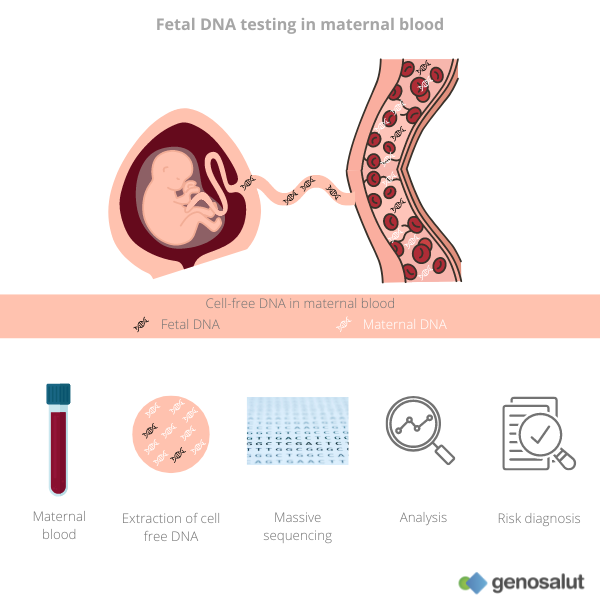
What is fetal DNA testing in maternal blood?
Fetal DNA testing, also known as non-invasive prenatal testing, is used to clarify some genetic diseases of the foetus from maternal blood. In particular, these foetal DNA tests are used to analyse the most common trisomies and numerical alterations of the sex chromosomes. In some cases they also detect other chromosomal abnormalities such as deletions.
What is cell-free DNA?
Tiny fragments of genetic material or DNA circulate in the blood plasma and other body fluids (cerebrospinal fluid, pleural fluid, saliva, etc.) of every human being.
In healthy individuals, most of this cell free DNA (cfDNA) in plasma originates from the haematopoietic system (responsible for the production of blood cells). However, in certain physiological or pathological conditions, such as pregnancy, organ transplantation and cancers, related/affected tissues may release DNA into the bloodstream.
What is fetal DNA?
Fetal DNA refers to DNA fragments from the placenta of the unborn child that circulate in the blood of pregnant women. This fetal DNA can represent up to ten percent of cell-free DNA.
When can fetal DNA testing be performed?
This non-invasive prenatal test can be done from the tenth week of pregnancy, the ideal time being between 12 and 14 weeks. The latest the test can be done is at the 24th week of pregnancy.
What diseases does the fetal DNA test detect?
Fetal DNA testing from maternal blood can predict with some probability (which will depend on the test) whether the baby has:
● Trisomy 21 (Down’s syndrome)
● Trisomy 18 (Edwards’ syndrome)
● Trisomy 13 (Patau’s syndrome)
Some tests can also provide information about fetal sex and the likelihood of having a sex chromosome aneuploidy:
● Klinefelter’s syndrome (XXY)
● Turner syndrome (X0)
● XYY syndrome
● Triple X syndrome (XXX)
Some fetal DNA tests, known as expanded tests, can also identify microdeletions, small losses in chromosomal material. Most microdeletions occur by chance, with no family history and no other risk factors such as maternal age. These syndromes are rare, i.e. they affect a very small percentage of the population and usually cause intellectual disability and malformations in different organs of the baby. They include:
● DiGeorge syndrome
● 1p36 Deletion Syndrome
● Angelman Syndrome
● Prader-Willi syndrome
● Cat’s meow syndrome (Cri-du-chat)
● Wolf-Hirschhorn syndrome
What are the advantages?
Fetal DNA testing is a simple, convenient, fast, safe and accurate technique.
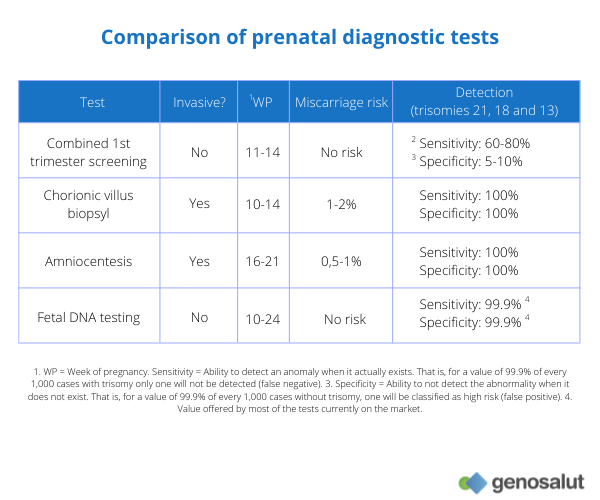
● It is safe because it is a non-invasive test, hence it is also known as non-invasive prenatal testing. It only requires a blood sample to be taken from the mother. In contrast, invasive tests such as amniocentesis (a puncture to take a sample of amniotic fluid) or chorion biopsy (a test to collect a sample of the membrane surrounding the placenta) pose a risk to the foetus, and have a 1% risk of miscarriage.
● It is simple and convenient because it requires only a blood sample to be taken.
● It is accurate because it detects the most common trisomies (Down’s, Patau’s and Edwards’) with a sensitivity and specificity of over 99.9%. These values are higher than those offered by combined first trimester screening, whose detection rate is lower (approx. 80%) and false positive rate (i.e. those unborn babies who according to the test are at high risk when in reality there is no chromosomopathy) is around 5%.
What are the disadvantages?
As mentioned above, it is a simple, safe and accurate test. However, it should be borne in mind that:
● It does not detect all chromosomal or genetic diseases. That is, a negative or low-risk result (no chromosomal abnormality detected) does not guarantee that the foetus is not affected by another genetic defect that is not analysed by the test. If there are results (usually ultrasound) that suggest that the baby may be at increased risk for other genetic defects, invasive testing (amniocentesis or chorionic villus sampling) is advisable.
● Despite its high reliability, it is a screening test and not a diagnostic test. This means that the results are expressed as probabilities and that any positive or high-risk result (detection of chromosomal abnormality) must be corroborated or ruled out by invasive testing (amniocentesis or chorionic villus sampling).
What are the differences with combined first trimester screening?
The differences relate to the procedure of the test, its reliability for trisomy detection and its coverage.
Test procedure
Combined screening requires:
● A maternal blood test, which studies two biochemical values: the beta fraction of the pregnancy hormone known as BHCG and the values of the pregnancy-associated placental protein or also known as PAPP-A.
● An ultrasound of the foetus, which dates gestation by measuring the cranio-caudal length (CRL) of the foetus, performs an anatomical study of the foetus and assesses markers (including nuchal translucency, the presence of nasal bone and the fronto-malar angle) associated with the risk of chromosomopathies.
The values obtained from the blood test and ultrasound are used to calculate the risk of trisomies 21, 18 and 13. A high-risk gestation is considered when the risk is greater than 1/250.
Fetal DNA testing only requires a maternal blood test.
Reliability of results
With regard to the reliability of the results, the fetal DNA test is more sensitive (has fewer false negatives) and more specific (has fewer false positives) than extended first trimester screening.
Coverage of the test
As far as chromosomal abnormalities are concerned, combined first trimester screening can only detect trisomies 21, 18 and 13. In contrast, the fetal DNA test can also detect sex chromosome aneuploidies and microdeletions, as well as determine foetal sex.
Fetal DNA testing and non-invasive prenatal testing – are they the same?
Yes, as mentioned above, they are the same test just called by different names.
What results can I get from the fetal DNA study?
The reporting of results varies depending on the laboratory. They can be reported as positive (detection of chromosomal abnormality) or negative (no chromosomal abnormality detected), as high or low risk for an abnormality, or as a probability.
As a general rule, most fetal DNA tests provide results for trisomy 21 (Down), 18 (Edwards) or Patau (13) or sex chromosome aneuploidies (Turner syndrome, Klinefelter syndrome, XYY syndrome and triple X syndrome).
● Low risk (or negative): the risk of the foetus having any of the above chromosomal abnormalities is unlikely but not excluded.
● High risk (or positive): the risk of the foetus having any of the above chromosomal abnormalities is high, but not yet certain. In this case, the result must be confirmed by invasive testing.
● Inconclusive: in some cases (between 1% and 5%) the technique is not able to provide a result. This is because it cannot clearly differentiate between maternal and foetal DNA and therefore cannot give a reliable result.
How reliable are the results?
The values for sensitivity (detecting the abnormality if it exists) and specificity (not detecting the abnormality if it does not exist) vary between providers. As a general rule, both are around 99.9% for trisomies 21, 18 and 13. That is, out of 1,000 cases with trisomy only one will be missed (false negative) and out of 1,000 cases without trisomy one will be classified as high risk (false positive).
For microdeletional syndromes the sensitivity is close to 74%.
How long does it take to get the results?
Generally, most laboratories have the tests available within 5 to 7 working days.
Who is the fetal DNA test recommended for?
Any woman who wishes to rule out the most frequent chromosomal alterations in her baby without putting her pregnancy at risk. However, it is especially indicated in the following cases:
● Women over 35 years of age, as the mother’s age is a factor to be taken into account in some chromosomal abnormalities such as Down’s syndrome or Edwards’ syndrome.
● Women at high risk of developing chromosomal abnormalities after first trimester screening.
● Women with previous pregnancies with Down’s syndrome or with detection of suspicious abnormalities on ultrasound.
The test can be performed in singleton and twin pregnancies (usually only trisomies 21, 18 and 23), in cases of pregnancy through in vitro fertilisation and assisted reproduction techniques, including egg donation and twin pregnancies.
In which cases is foetal DNA testing not recommended?
There are some specific cases in which the study of foetal DNA is not recommended, because they are situations that can alter the results. These are the following:
● Organ transplantation
● Blood transfusion (performed in the 3 months prior to the test)
● Stem cell treatments
● Previous abortion/miscarriage (within 6 months prior to testing)
● Oncology patients
● Heparin treatments
● Vanishing twin
● Overweight pregnant women
● Intense physical exercise shortly before the test
How much does it cost?
The price of the fetal DNA test depends on the laboratory and the coverage of the test, i.e. whether it only includes the analysis of autosomal trisomies (21, 18 and 13) or also the analysis of sex chromosome aneuploidies and microdeletions. It is usually between €400 and €750.
Does Spanish Social Security cover this test?
In some autonomous communities, such as Catalonia and Valencia, Spanish Social Security offers the test to pregnant women who meet certain criteria.
Does private insurance cover fetal DNA testing?
Most private insurance companies cover this non-invasive prenatal test for pregnant women who present a high risk in the first trimester screening.
At Genosalut we have been offering non invasive prenatal tests for more than 10 years. Our basic test analyses the most frequent trisomies (21, 18 and 13), sex chromosome aneuplodies and determines foetal sex. Our extended test also analyses various microdeletional syndromes.
If you like our blog, subscribe to our newsletter


