Prenatal genetic diagnosis
Our prenatal diagnostic tests
We are currently working on updating the website and we have more genetic tests available. If you do not find what you are looking for, please contact us through our contact form or call us on +34 616 59 01 65 from Monday to Friday from 9.00 am to 1.00 pm.
Why are Genosalut's prenatal genetic tests useful?
To find out as much information as possible about your baby's health
The different prenatal genetic tests available make it possible to detect with a high rate of accuracy (screening tests) or diagnose (diagnostic tests) chromosomal alterations or mutations in the baby that can cause mental and physical development disorders, malformations and complex syndromes.
To clarify doubts in at-risk cases
If there are hereditary diseases in the family, abnormal ultrasound findings, abnormal first trimester screening or a history of miscarriages in the patient or family, prenatal genetic testing is necessary.
To rule out genetic abnormalities that may have consequences for offspring
Some genetic errors have no consequences for the carrier, but may result in miscarriages or poor development and disabilities in the child.
What prenatal genetic tests do we offer at Genosalut?
At Genosalut we offer from non-invasive prenatal testing (NIPT) to exome diagnosis, always accompanied by genetic counselling. We treat each patient’s case individually and propose the best solutions for their specific situation.
Conventional prenatal genetic testing includes NIPT and chromosomal analysis. Extended prenatal genetic testing comprises single gene analysis, CHG array and exome analysis. These last three tests:
- They are recommended if an increased nuchal translucency or other foetal abnormality such as a heart defect, skeletal dysplasia or brain malformation is detected during ultrasound, or if there is evidence of a complex syndrome.
- They are intended to detect microdeletions and duplications, as well as mutations in individual genes, which are often the cause of complex malformation syndromes.
Non-invasive prenatal test (NIPT)
- Sample type: Maternal blood.
- Is it invasive? No.
- Technique: Massive sequencing.
- When is it recommended? Although there are several indications for non-invasive prenatal testing (high or moderate risk of foetal abnormality), it is important to note that any pregnant woman can be tested. The results obtained are highly reliable and can therefore be very reassuring for parents. The decision is a personal one and professional advice is important: just because a test is suitable for one woman, it does not mean that it is suitable for another.
- Purpose: Chromosomal disorders caused by chromosomal aneuploidies (extra or missing chromosomes), mainly Down’s syndrome, Edwards’ syndrome and Patau’s syndrome and sex chromosome aneuploidies.
It may include screening for other chromosomal disorders caused by missing (deletions) or duplicated fragments of a chromosome.
Conventional chromosome analysis (Karyotype)
- Sample type: Amniotic fluid or chorionic villi.
- Is it invasive? Yes.
- When is it recommended? When parents are carriers of rearrangements. Also to confirm suspected aneuploidy of chromosomes 21, 13, 18, X and Y detected by NIPT.
- Technique: Optical microscopy.
- Purpose: Detection of numerical chromosomal aberrations (aneuploidies such as monosomies and trisomies) and structural aberrations (such as deletions and duplications visible under the light microscope) of the 46 chromosomes with conventional chromosome analysis.
Single gene analysis
- Sample type: Amniotic fluid or chorionic villi.
- Is it invasive? Yes.
- When is it recommended? When criteria for extended prenatal testing are met and in addition there is a known severe familial inherited disease (e.g. spinal muscular atrophy or cystic fibrosis) or ultrasound findings point to a specific genetic defect.
- Technique: PCR and Sanger sequencing.
- Purpose: Targeted identification of mutations in individual genes.
Array CGH
- Sample type: Amniotic fluid or chorionic villi.
- Is it invasive? Yes.
- When is it recommended? When criteria for extended prenatal testing are met (abnormal ultrasound results) but chromosomal analysis is normal.
- Technique: Array CGH.
- Purpose: The entire genome is examined for microdeletions and duplications. In approximately 5-10% of pregnancies with abnormal ultrasound results and normal chromosomal analysis, array CGH can clarify the cause of the abnormal ultrasound results.
Exome/Genome
- Sample type: Amniotic fluid or chorionic villi.
- Is it invasive? Yes.
- When is it recommended? Severe malformations, such as a heart defect, skeletal dysplasia or brain malformation on ultrasound examination, or if there is evidence of a complex malformation syndrome. To check for pathogenic variants or mutations, parental blood is also examined.
- Technique: Exome/genome analysis by massive next generation sequencing (NGS).
- Purpose: Identification of mutations in the whole exome/genome that may be associated with the defects found.
Our value proposal
Experience
At Genosalut, we have more than 10 years of experience in counselling people with conditions where a genetic cause has been identified or is thought to be possible.
Proximity
We are a close laboratory, we respond personally and we take the time to explain the report in detail to doctors and patients.
Professional interpretation of results
Because of our knowledge and experience, we are able to accurately interpret genetic results and offer professional advice.
Reference in the field
We are the point of contact for patients, doctors and clinics in all areas of human genetic diagnostics and prevention.
Genetic counselling within the framework of prenatal diagnosis

In case of doubts, at Genosalut we solve them. During the previous genetic counselling session we talk to patients about the possibilities and limitations of the different prenatal diagnosis tests.
We clarify your doubts
We take into account the results of different medical tests
We take into account your personal and family history
We assess genetic risks
We discuss the importance of all the information for your life and family planning
Once the results have been obtained, we detail their significance and the consequences that may result from them. We discuss with patients the possibilities of support in case of physical and psychological stress caused by the result.
FAQs
What is prenatal testing?
It is a set of tests performed before or during pregnancy to try to monitor the correct development of the foetus and rule out the presence of possible congenital defects and also to determine the presence of maternal risk factors. These tests, both screening and diagnostic, can be invasive or non-invasive. These include: carrier analysis, first trimester screening, morphological ultrasound, non-invasive prenatal testing, karyotyping, panels and exome.
What is prenatal genetic testing?
Prenatal genetic diagnosis comprises a series of genetic and molecular techniques that allow us to examine the genetic material of the future parents and/or foetus.
Our genetic material is contained in chromosomes, thread-like structures inside the cell nucleus. Our approximately 20,000 genes, most of which we have in duplicate, are distributed over 23 pairs of chromosomes. Consequently, each of our cell nuclei contains 46 chromosomes.
Changes in genetic material can lead to mental and physical developmental disorders, malformations or complex syndromes. These can be changes in the number and structure of chromosomes or changes (mutations) in individual genes.
With prenatal genetic diagnosis, the genetic material of the foetus can be examined for possible changes. There are several methods that can be used depending on the question, the patient’s own or family history and the need for certainty.
In which situations is prenatal genetic diagnosis recommended?
Although most pregnancies go without problems or complications, there are situations in which prenatal genetic diagnosis is necessary to identify risks in time or to clear up justified doubts and concerns. It is especially important in the case of:
- Inherited diseases in the family
- Abnormal screening in the first trimester or abnormal ultrasound findings
- In case of a history of miscarriages in the patient or the family
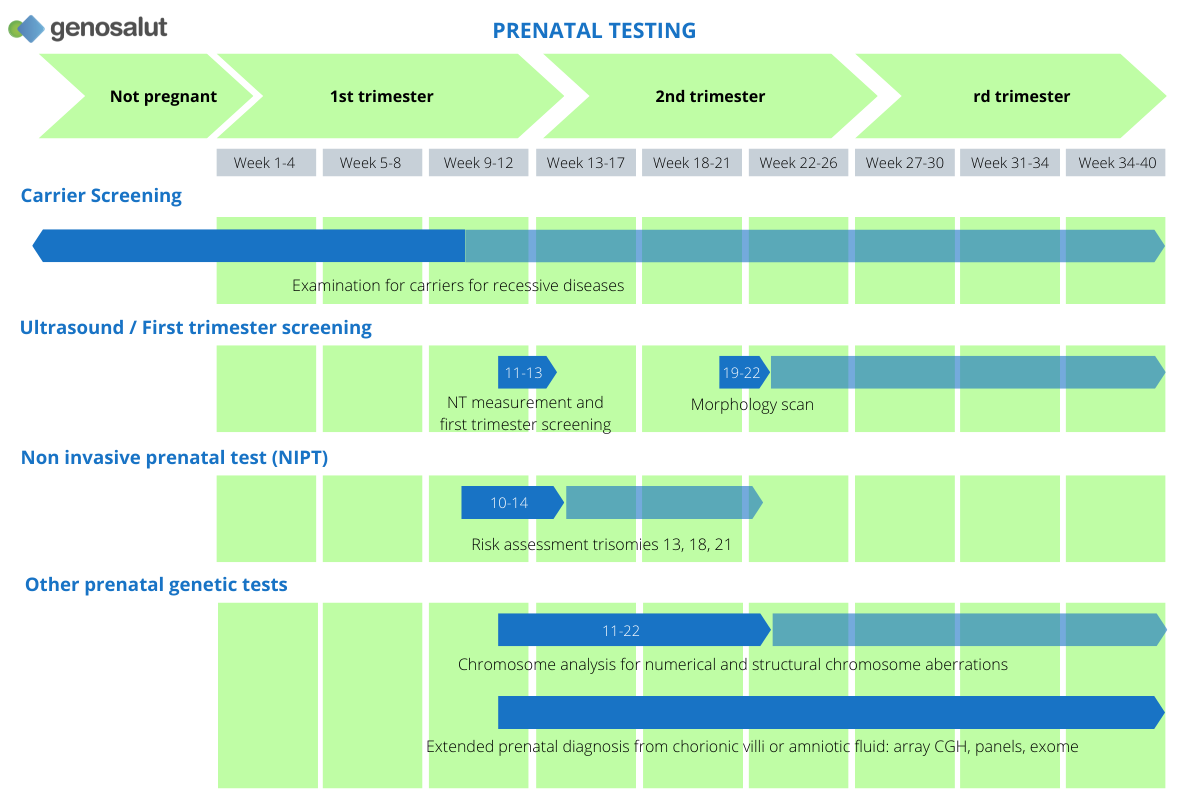
When can the different prenatal genetic tests be performed?
The type of diagnostic test and the timing will depend on each individual case. As a general rule:
- Before pregnancy: Either because of a history or because of a desire for greater certainty, one or both partners can undergo testing before pregnancy. Depending on the circumstances, it is advisable to carry out: a single gene analysis or a carrier genetic study to detect predisposition to severe recessive diseases.
- Early pregnancy: A non-invasive prenatal test from maternal blood is possible as early as the tenth week of pregnancy.
- Late pregnancy: If more certainty is required or if there are abnormalities in the ultrasound scan, an extended full genetic diagnosis can be performed. It is used to detect chromosomal alterations and mutations in individual genes.
What prenatal genetic diagnosis techniques are available?
- Non-invasive prenatal test: Allows highly accurate determination of numerical chromosomal abnormalities (mainly of chromosomes 13, 18, 21, X and Y).
- Chromosome analysis (karyotyping): Allows the identification of chromosomes in the dividing cell after staining, determining chromosome number and structure. This technique can be used to detect numerical chromosomal abnormalities (as in Down’s syndrome) and large structural chromosomal abnormalities.
- Array CGH: Allows the detection of small structural chromosomal abnormalities such as those found in several microdeletion and microduplication syndromes (DiGeorge syndrome, ngelman syndrome, Prader-Willi syndrome, Williams syndrome).
- Single gene analysis: Allows the identification of specific mutations in individual genes. This test is advised if there is a family history of an inherited disease (cystic fibrosis, spinal muscular atrophy…) or if ultrasound examination indicates a specific genetic defect.
- Exome analysis: The whole exome can be examined in a single test. It is a useful test if severe malformations (heart defects, skeletal dysplasias or brain malformations) are detected on ultrasound or if there is evidence of a complex syndrome.
These tests are sometimes also classified as follows:
- Cytogenetic: Those aimed at identifying alterations in the structure of chromosomes. These studies include: karyotyping and array CGH.
- Molecular: These allow the identification of point mutations in a gene or specific genes. They can be used to detect specific mutations (usually by Sanger sequencing) or to detect alterations in multiple genes simultaneously by next-generation sequencing (NGS).
What are the objectives of prenatal genetic testing?
Prenatal genetic testing allows the detection or exclusion of risks and genetic diseases in the foetus at an early or later stage. Even complex prenatal clinical pictures, sometimes associated with multiple malformations, can be diagnosed prenatally.
What are genetic diseases?
Genetic diseases are caused by changes in a person’s genes or chromosomes. We speak of aneuploidy when there are extra or missing chromosomes. In a trisomy, there is an extra chromosome. In a monosomy, one chromosome is missing.
Monogenic diseases are caused by changes in genes, these changes are called mutations. Monogenic diseases include sickle cell anaemia, cystic fibrosis, Tay-Sachs disease and many others. In most cases these are recessive diseases, so both parents must carry a mutation in the same gene to have an affected child.
There are also genetic diseases caused by chemical modifications of the DNA sequence (epimutations).
What is an array CGH and when is it recommended for prenatal diagnosis?
Array CGH is an accurate genetic technique for prenatal diagnosis of very small changes in genetic material that are not detected by karyotyping. These changes can be: microdeletions (absence of a very small piece of chromosome) and microduplications (addition of a piece of chromosome). Both defects can cause diseases that affect the intellectual and physical development of carriers. It does not identify point mutations or chromosomal alterations in equilibrium (balanced translocations).
An array CGH requires an amniocentesis or chorionic villus sampling to obtain the necessary sample (amniotic fluid or chorionic villi, respectively). An array CGH is especially recommended if:
- Abnormal findings are observed on ultrasound: organ malformation in combination with growth retardation or multiple malformations.
- If there are abnormal chromosomal findings that need to be further clarified.
- If the prospective parents have a great need for reassurance and want very detailed information about the chromosomal picture of the foetus.
What is an exome and when is it recommended for prenatal diagnosis?
Exome sequencing is a technique that allows a large number of genes to be analysed by massive next-generation sequencing.
Imaging methods sometimes provide inconclusive information. In the following doubtful cases, fetal exome testing is recommended:
- Cardiac defects
- Skeletal dysplasia
- Brain malformations
- Indications of a complex syndrome
As for an array CGH, amniocentesis or chorionic villus sampling is required to obtain the necessary sample.
Which prenatal genetic diagnosis technique is the most recommended?
There is no one better than the other, the decision depends largely on:
- The question to be answered
- The time of the pregnancy
- Family history
- Possible anomalies in the ultrasound scan
- The individual need for security of the parents-to-be
What are the differences between non-invasive and invasive prenatal testing?
Prenatal diagnostic techniques are usually divided into two broad categories: non-invasive prenatal diagnosis and invasive prenatal diagnosis.
Non-invasive prenatal testing (NIPT)
No invasion of the foetal environment is required.
- Sample: Mother’s blood. Modern, highly sensitive methods detect small amounts of fragments of the child’s genetic material in the pregnant woman’s blood (cell-free foetal DNA).
- At what point in pregnancy should a non-invasive prenatal test be performed? This type of test can be performed from the 10th week of pregnancy and generally before the 22nd week, which is the limit for legal termination of pregnancy in Spain, subject to a medical diagnosis that justifies it.
- What is analysed? They compare maternal and foetal DNA to detect whether the foetus has a high risk of suffering from a chromosomal disorder. It is usually limited to the detection of trisomies 21, 13, 18, X and Y.
Invasive prenatal diagnostic methods
Invasion of the foetal environment is necessary. Amniocentesis consists of the extraction of amniotic fluid (where fetal cells are found) through puncture of the maternal abdomen, and chorionic biopsy, consists of the collection of placental tissue via the transcervical route.
Sample: Amniotic fluid (amniocentesis) and chorionic villi (chorionic villus sampling).
At what point in pregnancy should an invasive prenatal test be performed? As these tests are usually usually linked to suspicious NIPT or abnormal ultrasound findings, they are usually performed between the 12th and 22nd week of pregnancy.
What do they analyse? There are different techniques to analyse the sample obtained. The purpose is to detect genetic or chromosomal abnormalities before the foetus is born.
Who covers the costs of prenatal genetic diagnosis and counselling?
As a general rule, genetic counselling is not covered by any type of health insurance.
As far as prenatal genetic testing is concerned, it is covered by some private insurance companies and sometimes depends on certain criteria (patient’s medical history, family history, etc.). You can come to us with a certificate from your gynaecologist or with your insurance card.
Request an appointment with us
Opening hours
Monday to Friday from 9.00 am to 1.00 pm
+34 616 59 01 65
info@genosalut.com
Camí dels Reis, 308 (Clínica Palma Planas)
Contact form
Reasons for trusting Genosalut
First genetic diagnosis laboratory in the Balearic Islands
Professionals with experience in medical genetics
Detailed report of the results
Personalised attention for each patient
Wide range of genetic tests
Cutting-edge technology
